CMV and pregnancy
You can find all information about CMV infection during pregnancy using the Q&A below.
What is CMV
Cytomegalovirus is a member of the herpes virus family. It is the most common congenital infection in the Western world. 1.5% of newborn babies have CMV, so it is much more common than toxoplasmosis, spina bifida or Down syndrome.
An infection with (CMV) is common and usually harmless. As an adult, you will at most show some cold-like or flu-like symptoms. But for the unborn child, the virus can have serious consequences. Symptoms can vary from hearing loss to serious developmental and motoric delays.
When am I at risk?
Not everyone is at serious risk of CMV infection. If you have had CMV before and have therefore produced antibodies, you are much less likely to pass the virus on to your child.
But if this is the first infection - a 'primary infection' - occurring early in pregnancy , then the virus is passed on to the fetus in 1 out of 3 cases. During this first infection your body builds antibodies against CMV. Such a primary infection later in pregnancy is passed on in 60-70% but is rarely harmful to the fetus at that time.
The virus remains dormant in your body after healing and can reactivate later. When and why this happens is still unclear. In addition, it is also possible to be infected with a second CMV strain. We call these 'secondary infections', antibodies are already present and the risk of passing on the virus during pregnancy is < 2%.
The virus mainly occurs in young children between the ages of 2 and 3. Mothers who already have a child or who regularly come into contact with small children are therefore at higher risk .
How can I prevent a CMV infection?
CMV is transmitted through contact with various bodily fluids such as saliva, stool, urine, breast milk, blood and during sexual contact.
To prevent you from becoming infected with CMV during your pregnancy, it is important to follow the following advice as closely as possible throughout your pregnancy, but ESPECIALLY in the first trimester :
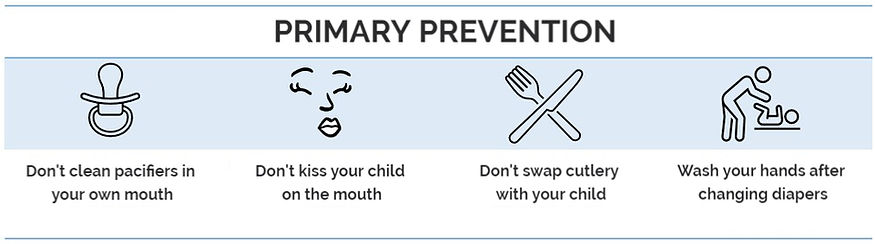
If you do not have antibodies to CMV yet, these measures are EXTREMELY important . We can detect the presence of antibodies in your blood.
How do I know if I am infected?
We can detect a primary infection in your blood.
With two consecutive blood samples we can detect if you recently contracted a primary infection. It is best to have this checked when you are planning to become pregnant: only then will the test be reimbursed.
When you are pregnant, it is very useful to check your antibodies during the first trimester (< 14 weeks). Unfortunately, this test is not (yet) reimbursed and costs an average of 2x17 euros.
When antibodies are already present, a secondary infection is still possible; we cannot detect this. Fortunately, a secondary infection is rarely passed on to your baby.
How do I know if my baby is infected?
If we detect a primary CMV infection at the beginning of your pregnancy, your GP or gynaecologist will refer you to a perinatal centre for an extensive discussion about the risks, possible treatment and further diagnosis and care. There is a 1 in 3 chance that the infection will reach the foetus via the placenta .
The diagnosis of a fetal infection can be checked with great accuracy and very limited risk with an amniocentesis . If no DNA of the CMV virus is found in the amniotic fluid, this is very reassuring and the baby is NOT at risk of serious consequences.
A contamination in the amniotic fluid does not mean that the baby will show serious consequences of this infection. Only 1 in 3 children develop consequences, 65% show no symptoms at all. In case of an amniocentesis that is positive for CMV, you will be regularly monitored during the rest of the pregnancy with specialized ultrasound and an MRI scan .
Is there a treatment?
If we discover serious damage to the fetus on ultrasound due to a CMV infection, we cannot offer treatment. Termination of pregnancy may be one of the options in the event of very serious damage.
With a milder degree of damage, Valganciclovir can be started after birth to slow down hearing loss. This medication has side effects, so the pros and cons are carefully weighed by the pediatrician.
Treating CMV during pregnancy is not possible, which is why we try to prevent the virus from reaching the fetus through medication. Recent studies have shown that the risk of transmitting CMV to the fetus is reduced by 66% after treatment with Valaciclovir, an antiviral drug. Valaciclovir is a well-known medication, but it is not yet reimbursed for CMV infections during pregnancy. More research is needed into its effectiveness and safety.
This data was collected in the TreatCMV study, a study conducted across seven Flemish hospitals where patients with a CMV infection in early pregnancy where treated with Valaciclovir between July 2024 and July 2025. Here too, a significant reduction in the number of CMV infections in the fetus was observed. Therefore, we recommend that patients with an early CMV infection start Valaciclovir, this treatment is usually started in one of the seven referral hospitals (see 'The Research Team').
This means you will need to take 8 grams of Valaciclovir per day for a minimum of 8 weeks. Please note, the medication only comes in 500 mg tablets, so that’s 4 x 4 tablets per day, with a total cost of approximately €500–750. About half of patients experience mild side effects such as nausea, vomiting, diarrhea, abdominal cramps, headaches, or fatigue. In 1 in 100 cases, acute kidney failure is observed, which fully recovers after stopping the treatment. For this reason, regular blood tests will be performed to monitor kidney function. After eight weeks of treatment, and if you are at least 18 weeks pregnant, the treatment is stopped. At that time, your doctor will perform an amniocentesis to check whether CMV was still transmitted. The further follow-up of your pregnancy will be organized based on this result.
The TreatCMV study is still ongoing but is no longer accepting new patients. Read more below about the design of the study:
TreatCMV study
Seven Flemish perinatal hospitals are working together to demonstrate the prevention of CMV through Valaciclovir. Our goal is to increase awareness of CMV among pregnant women, to offer standardized screening (detecting antibodies in mom's blood) and to start Valaciclovir when a CMV infection is diagnosed during screening.
All study patients with a primary, first trimester CMV infection received Valaciclovir 4x4 tablets per day from the time of confirmation of the infection until the time of amniocentesis (around 20 weeks of pregnancy) to prevent the transmission of the infection to the fetus. After at least 8 weeks of treatment, an amniocentesis was performed to detect CMV in the amniotic fluid. Afterwards the pregnancy was followed with detailed ultrasound examinations and an MRI examination.
After birth the baby is tested for CMV (urine analysis, blood tests, brain ultrasound and an MRI).
To ensure all examinations run smoothly, the delivery takes place in one of the seven participating hospitals.
A yearly follow-up is organized until the age of 5, to continue to monitor hearing and brain function in the long term.
What happens after birth?
A child with CMV is closely monitored in Flanders thanks to a strong network of pediatricians, ENT doctors, neurologists, ... . A follow-up trajectory is mapped out for your child, which is led by the COS ( center for developmental disorders ). For more information, we refer you to the website https://cmvreg.be/information-for-patients/.
Are you a parent of a child with CMV? Or are you, as future parents, looking for more information from couples who went through a similar situation? Then definitely visit the website of the parent group Care4CMV at https://care4cmv.be/
